Linda Brown has run support groups for people with unseen illness. When she heard the list of symptoms for people experiencing Long COVID, she thought they sounded similar to those listed by people living with ME/CFS (chronic fatigue).
WTIU News, Bente BouthierThough deaths and hospitalizations for COVID-19 infections have stabilized, the Centers for Disease Control says as many as 4 million Americans are living with Long COVID.
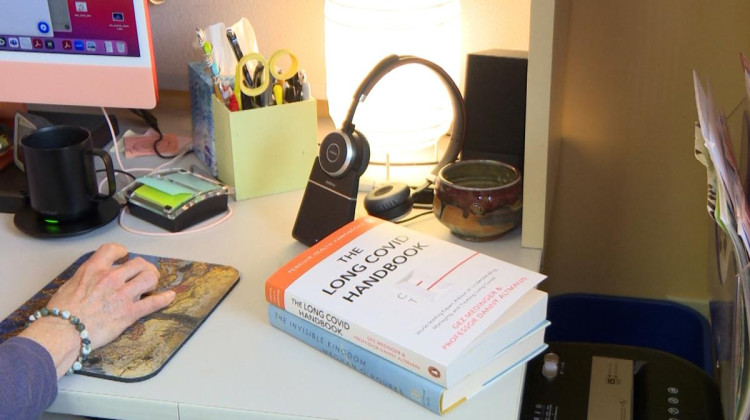
Bloomington clinical health psychologist Linda Brown has treated people with unseen illnesses for years. She saw reports of COVID-19 infections and persisting symptoms in 2021.
Since March 2020, more than 1.8 million Hoosiers have tested positive for COVID-19, according to the Regenstrief COVID Dashboard. In that time frame, more than 33,000 of those cases came from Monroe County.
“I thought, ‘Oh, wow, if the numbers are going to be like that, they're going to be really big here in Indiana. And maybe a group like the group that I've been running for women with invisible illness will be needed.’”
She started an online group for people living with Long COVID this year, teaching patients to advocate for themselves and to use energy management techniques.
Read more: Holcomb signs letter urging Biden to end public health emergency
The US Department of Health issued guidance that Long COVID can be a disability under the Americans with Disabilities Act. But Brown said not everyone has access to the health care they need to start making a recovery.
She said in some cases when her patients told their doctors about lingering COVID symptoms, they were met with skepticism.
“(Doctors) said, ‘Oh, I'm not really finding that to be a thing.’ And of course, that was devastating to the person I was working with, because he was suffering.”
Suzie Smith is one of Brown’s patients. She had to stop working after her second bout of COVID. Since 2021, she’s had shingles twice, Bell’s Palsy, extreme fatigue, and seizures.
Read more: Long COVID patients join a chronic illness community seeking answers
“And nobody was talking about Long COVID yet," Smith said. "But I was having these bouts of fatigue that were keeping me out of work for a couple of days at a time.”
That was huge for Smith, who used to juggle work at a law firm, exercise, and take care of five kids. She got her law degree from IUPUI in 2017, at 33 years old, and wasn’t ready to put her career on hold.
Because of the seizures, Smith hasn’t driven since August 2021.
"I'm supposed to be the caregiver. I'm supposed to be the one that does everything. And so it's really, really hard."
She and her family kept looking for answers. But ready access to doctors and treatments aren’t quickly available in Ladoga, where she lives.
"So it took from all of 2021 until about November, when they started popping up with these Long COVID clinics," she said. "And I was like, I need to get into one of those. I need to see if that's what's going on.”
At Cleveland Clinic in 2022, she was diagnosed with chronic fatigue syndrome, which her neurologist said is a result of COVID.
From there, she was connected with Brown's online support group.
“It helped me to understand I have a baseline," Smith said. "And if I push, it's like these illnesses push right back at you.”
Now she stays home, doing some chores when she’s able. Her seizures have subsided some since and she has an internal medicine specialist she trusts.
Read more: Regenstrief launches study on Long COVID
Another of Brown’s patients, Yvonne Thompson, also had to stop working in education after she got COVID in October 2020. She tried to return to work initially, a few weeks after getting sick.
"And I remember my first day back to work, I was driving on the south side of Indianapolis and feeling like I couldn't breathe and my heart was pounding," Thompson said. "And I got to work and long story short, those symptoms just got worse and worse and worse. As the weeks went on, I had trouble going upstairs. My heart rate would just out of nowhere, get erratic, and I just had this horrible fatigue."
A cardiologist diagnosed her with Postural Orthostatic Tachycardia Syndrome.
Thompson is grateful her physician took her seriously and that she was able to access specialists to help her get better. She had to devote herself to decreasing inflammation in her body: eating on a strict diet and limiting her social and workloads.
Now, Thompson can work part time.
Thompson and Smith describe themselves as caretakers and community members who were always on the go before.
Thompson said mental health counseling with Brown was essential to her treatment, dealing with the PTSD and grief that came with her illness. She thought PTSD just affected people who had served in combat or been victims of terrible crimes.
"There's some stigma attached to saying, 'Oh, you have PTSD, because of a virus.' And it's not like an event that caused the PTSD. It's the actual physiological impact this virus had on my body and my brain that caused this response. And I had a hard time wrapping my mind around that.”
Smith wants treatment to be more personalized to Long COVID's wide range of symptoms.
Brown said more multidisciplinary clinics should open, so that people living with Long COVID don’t have to seek treatment so many different places.
It may be helpful if everyone is aware that there may be people in their social circles, who are silently living with Long COVID," she said. "What to do about that? I'm not sure other than be as open as possible to talking to people who have had COVID and are reporting lingering symptoms, otherwise, I think we're still figuring out how to deal with this."
She’s got a second round of the therapy group going now with seven members and will be taking more patients for a third round in September.
 DONATE
DONATE






 Support WFYI. We can't do it without you.
Support WFYI. We can't do it without you.