Content warning: This story includes detailed descriptions of psychiatric hospitalization, involuntary confinement and allegations of medical neglect.
Tina Blackburn woke up in her rental car outside the locked doors of Medical Behavioral Hospital of Indianapolis in Greenwood, Indiana. Inside was her 35-year-old daughter, Jessica Ravellette.
Ravellette was a hundred miles from home when she arrived — delirious, "unable to keep eyes open consistently," medical records documented. She'd been transferred from her local hospital after she had surgery on an abscess on her arm.
Blackburn couldn't understand why her daughter — who needed medical treatment for her arm — was in a psychiatric hospital at all. She traveled here to get answers.
When Blackburn finally saw her daughter, she was alarmed. Ravellette couldn't form a sentence, Blackburn said. Ravellette's arm was swollen and draining fluid and her temperature had spiked to more than 102 degrees, medical records show.
She wanted her transferred out to recover at a regular hospital, but was told that Ravellette was held under an emergency detention order — a legal process that allows hospitals to keep patients for up to 14 days if a judge finds they're mentally ill, dangerous, or unable to care for themselves.
For more than three days in June 2024, Blackburn pleaded with staff to release her daughter. When nothing changed, she went to the Greenwood Police Department.
Later that day, an officer walked into the hospital with Blackburn and asked hospital staff to show the court order authorizing Ravellette's detention.
"It was supposed to go through court, but I guess it never went through a court," the officer said about Ravellette's detention order. "So we're trying to figure out if she's eligible to leave, or why she isn't eligible to leave, or what's going on."
Then, staff confirmed several times that the court never approved the detention order, according to body-worn camera footage obtained by WFYI.
And the next day, Ravellette was released — ending seven days at the hospital.
"That was the scariest place I've ever been," Ravellette said. "I thought I was either going to die there or wake up without my arm."

The hospital is part of NeuroPsychiatric Hospitals, a for-profit psychiatric hospital chain based in Indiana with locations in Indiana, Texas, Arizona and Michigan. The company takes patients with both medical and psychiatric needs — people who many hospitals refuse or can't care for. With few hospitals like it in some regions, patients in other states are sometimes transferred to its facilities.
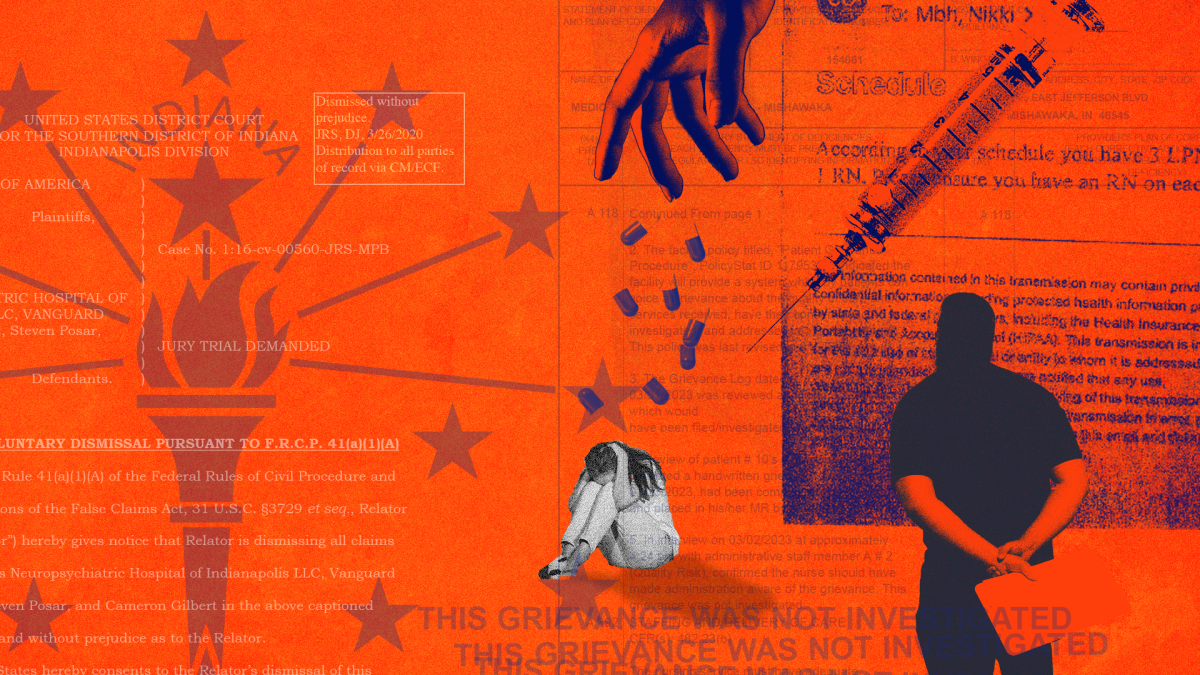
WFYI interviewed more than 40 former patients, relatives, staff and experts who described a hospital system that strands vulnerable people with little recourse. Their accounts — corroborated by lawsuits, medical records and hundreds of state and federal inspection reports — show NeuroPsychiatric Hospitals was repeatedly cited for serious violations, including the federal government's most serious warning, and was the subject of hundreds of substantiated complaints over the past decade.
Inspection records, lawsuits and interviews describe patients left unattended for hours, units so short-staffed that basic care was missed, and others transferred to emergency rooms in such critical condition that doctors told WFYI they questioned how the patients were still alive.
Despite repeated violations, regulators imposed few lasting penalties — often cutting private deals instead.
The company declined to comment on individual patient cases, including Ravellette's. NeuroPsychiatric Hospitals said discharge decisions are based on independent decisions by clinicians and that it endeavors to operate under strict adherence to applicable federal and state detention laws, adding that federal rules require hospitals to develop discharge plans outlining where patients will go and how their care will continue after leaving the facility.
Michael McNally, the chain's attorney, acknowledged the existence of substantiated complaints but said a new leadership team installed in 2022 made systemic improvements.
"I'm not ever going to say that there's no complaint that could be substantiated — that would be ignorant," McNally said. "My experience: nothing's ever perfect."
He added that the hospital submits plans of correction when regulators identify problems.
Asked about complaints from patients, families, and staff, as well as hundreds of regulatory deficiencies, McNally defended the company, saying few other hospitals are equipped to treat patients with both medical and psychiatric needs.
"They don't really have anywhere to go," McNally said. "Even if we ran the crappiest facility possible, it's probably either going to be on par with or slightly better than the next alternative."
1 — The ascent
Like many other states, Indiana had long struggled to care for people with both psychiatric illnesses and complex medical needs — patients too sick for psychiatric wards, yet too unstable for medical floors.
NeuroPsychiatric Hospitals set out to fill the void.
Cameron Gilbert founded NeuroPsychiatric Hospitals in 2006, presenting it as the answer to one of medicine's hardest problems: what to do with people with both psychiatric illness and complex medical needs. In a public biography of Gilbert, NPH patients were described as "the worst of the worst." Christy Gilbert, his wife, was the company's president and chief operating officer. Together they steered the chain's early growth.
But in 2013, the Centers for Medicare & Medicaid Services and the Indiana Department of Health cited the chain's first hospital, in Bremen, for serious lapses in patient care, record-keeping and safety. Inspectors found patients left without critical lab results for hours, staff unable to demonstrate training in restraints and seclusion, and missing medication records. An inspection also found a patient whose infection went untreated for days before being transferred to another hospital, where they later died, likely due to sepsis, according to the inspection records. "Medical staff rules and regulations are not being adhered to," inspectors wrote.
And according to a 2016 federal False Claims Act complaint filed by a former nurse practitioner in 2015, Gilbert gathered staff at the newly opened Indianapolis hospital and told them no one should be discharged before 14 days — regardless of a patient's condition. At that time, state law capped involuntary detainment at 10 days.
The lawsuit alleged that NeuroPsychiatric Hospital of Indianapolis used the so-called 14-day "holding policy" to maximize Medicare payments. That would violate federal rules that require psychiatric hospital care to be medically necessary and actively treating a patient's condition.
Gilbert allegedly told staff, "Fourteen days is the money maker," describing the billing "sweet spot" as 14 to 17 days and requiring his personal approval for any discharge.
Cameron Gilbert, who no longer holds any role with the hospital, did not respond to repeated requests for comment over several months.
The nurse practitioner further alleged she was suspended after she discharged a female patient who was frightened by men wandering into her room, according to court filings.
The lawsuit was later withdrawn. Michael McNally, the attorney for NeuroPsychiatric Hospitals, said the allegations are false. "In the lawsuit, and to this day, NPH has denied the allegations as being without merit," he said.
The nurse practitioner who filed the fraud claim against NeuroPsychiatric Hospital of Indianapolis spoke with WFYI but requested anonymity because she still works in health care and fears professional repercussions.
She said she still worries about the patients left inside.
"It felt like a movie," she said about her time at the hospital. "You don't think these types of people exist, and they do."
"But I don't have the money or the resources to fight it."
In the years that followed, state lawmakers expanded hospitals' power to detain psychiatric patients from 10 to 14 days under emergency detention orders — not counting weekends or holidays — if they're mentally ill, dangerous or gravely disabled or in immediate need of hospitalization and treatment.
Indiana Disability Rights, the state's federally authorized watchdog for people with disabilities, opposed the change in 2023, warning that expanding detention powers without stronger safeguards could increase the risk of abuse.
"While that provider is hopefully the exception rather than the rule," Executive Director Melissa Keyes wrote in a letter to state lawmakers, "there remains significant concern for abuses."
Indiana Disability Rights did not name any specific provider in the letter.
2 — The oversight
As employees and families continued to raise alarms in the years after the lawsuit, regulators conducted overlapping investigations and found a trail of violations — the chain pushed back on oversight.
In 2017, Indiana health officials tried to revoke the Indianapolis hospital's license, saying it failed to keep patients safe — for allegations that included not verifying prescriptions, poor recordkeeping and breaches of confidentiality.
The hospital chain sued to block the action. The case ended in a 2020 settlement with terms that were not made public. The Indiana Division of Mental Health and Addiction did not respond to WFYI's repeated requests for comment.
In 2018, Indiana Disability Rights attempted to conduct monitoring visits at the Indianapolis location. The group holds federal authority to monitor psychiatric facilities. Again, the company sued. It accused the watchdog group of harassment and argued it had no authority to press for access to the facilities. Court records show the case ended in a private settlement. Indiana Disability Rights said it cannot speak publicly about the case due to the settlement terms.
In 2020, federal inspectors found serious safety lapses at the Indianapolis hospital. At least four patients died during a four-month period. Inspectors declared the hospital in "immediate jeopardy" — what CMS refers to as the "most serious deficiency type," used when patients face an imminent risk of harm or death.
Inspectors cited dangerous infection-control failures during the first wave of COVID-19, including not keeping patients isolated while awaiting test results. According to inspection records, the hospital submitted a corrective plan. The order was lifted the same day.
Not long after, the chain attracted a new investor — Enhanced Healthcare Partners, a private equity firm that buys and expands health care companies. The terms of the deal were not disclosed, and Enhanced Healthcare Partners did not respond to requests for comment.
By 2022, NeuroPsychiatric Hospitals had replaced its executive leadership team — a shift its attorney described as part of a broader effort to reform operations. Some of the new leaders came from Acadia Healthcare, a chain The New York Times later reported held patients against their will to maximize insurance payouts.

McNally said the new team has "implemented significant corrective actions and systemic improvements."
The company says it also boosted staffing and strengthened oversight since 2022. The chain continues to deny that patients have ever been held for financial reasons and insists that all care decisions are based solely on clinical need.
Casey Webber, the hospital chain's director of patient experience, told WFYI in an October interview that behavioral health facilities like NeuroPsychiatric Hospitals are "wildly understaffed and underfunded," struggling to meet the overwhelming need.
His job, he said, is to listen — to collect patient surveys, field calls from families and make sure "everyone is treated with respect and dignity, and no one falls through the cracks."
"We're here for our patients," Webber said. "And in the midst of all the noise, I believe we do good work."
3 — The resistance
Today, the chain operates at least 400 beds nationwide. Medicare cost reports show it reported more than $76 million in net patient revenue, with over 6,700 discharges in the most recent filings.
Across Indiana, many psychiatric providers agree on the need for hospitals willing to take patients that most facilities refuse — people with both medical and psychiatric needs. But some told WFYI they face an ethical dilemma: they believe some patients are at greater risk inside NeuroPsychiatric Hospitals than they would be on the street.
"They don't have the staff, the facilities, or the ability to care for anyone," said Tim Templin, a board-certified behavior analyst who started in 2020 at the chain's Mishawaka and Bremen facilities.
"They make it seem like they can take anybody," Templin said. "But they can't."
Psychiatrists who reviewed patient records at the request of WFYI said they found problems, including vague notes, recycled language and little medical justification for prolonged stays. In one file, a patient's chart even contained another patient's records.
A dozen former staff — registered nurses, behavioral health technicians and supervisors — spoke with WFYI, granted anonymity because they feared retaliation. Many told WFYI they witnessed prolonged detentions. Several, after moving to new employers, said they quietly intervened to stop transfers to NeuroPsychiatric Hospitals.
Two attending psychiatrists in Indiana said they had repeatedly received transfers from NeuroPsychiatric Hospitals in dire shape, often with scant documentation after weeks inside. They said they didn't know how some of these patients were alive. They joined others who told WFYI they tried to limit any transfers to NeuroPsychiatric Hospitals' facilities.
One requested anonymity because he feared speaking publicly could compromise his clinical work. He said patients often arrived in the worst condition he had ever seen — and pleaded with him not to send them back.
The second requested anonymity because of fear of retaliation from the hospital chain. She said she warned the company directly: "This is not safe. You are harming patients."

More than a year after she was released, Jessica Ravellette has moved into a new home and settled into therapy, but said she thinks about her experience all the time.
She said it was traumatic to be stuck somewhere she couldn't leave, not knowing why she was there.
"I felt so helpless," Ravellette said. "I just don't want it to happen to anybody ever."
Farrah Anderson is an investigative health reporter with WFYI and Side Effects Public Media. You can follow her on X at @farrahsoa or by email at fanderson@wfyi.org
 DONATE
DONATE







 Support WFYI. We can't do it without you.
Support WFYI. We can't do it without you.