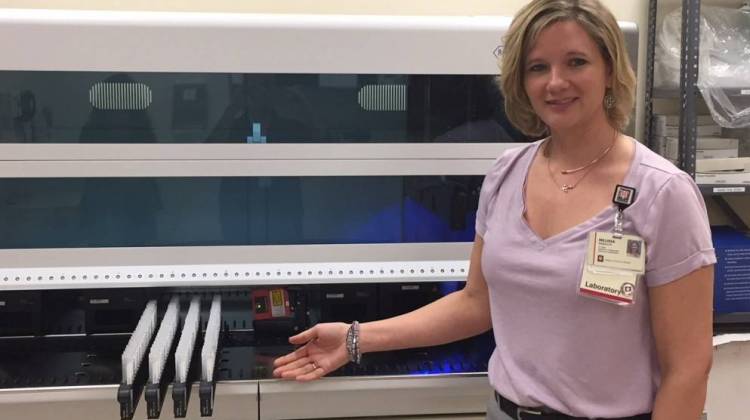
Melissa Randolph, cytopathology supervisor at Indiana University Health, shows a new piece of equipment in the lab.
Jill Sheridan/IPB NewsIndiana University Health is now providing genetic screenings to identify high risk strains of the human papillomavirus or HPV that causes cervical cancer. About 250 Hoosier women are diagnosed with this cancer every year.
Cytopathologist Melissa Randolph explains to Indiana Public Broadcasting’s Jill Sheridan how the screenings work and who they benefit.
We knew that were a lot of different strains of HPV, but there are really 14 different high risk types that we’re paying attention to right now. And two of those types are the ones that lead to 70 percent of our cervical cancer cases – at least that we know at this time.
How long have you known about those high-risk types?
This is definitely something that’s advancing. It’s been about five years, that it’s taken genotyping to kind of catch on. And people really didn’t know what to do with all the information at first. But what it’s teaching us is that there are certain patients that need to proceed to a colposcopy procedure to make sure that they really have any kind of precancerous changes that could be taken care of very quickly.
Talk about that, what is genotyping?
So genotyping, is actually a way, after we decide the patient carries a high-risk HPV virus, so we know a patient carries a 16 or 18, which are the high risk types that are most likely to lead to cervical cancer, or there are 12 other high risk types. Those patients still may be at a somewhat of a risk for cervical cancer, but less so than the ones who have a 16 or 18 genotype. So that’s how we’re using that information to help now.
And here at IU Health, you’re streamlining that screening process. Explain how that happened.
So, we’ve actually gotten to the point, where when a patient presents for cervical cancer screening, they’re going to get a pap test, we’re going to be able to look at their cells, and be able to see if they’re carrying any kind of lesion. We’re also going to be able to tell them whether or not they’re carrying a high-risk HPV virus, and then if they are carrying that virus, which one.
Now what, the important thing about this is, is that there HPV is so rampant in the population anyway. So what we want to do, is not scare anybody who is in an age group that they’re not likely to get cervical cancer. We don’t want to over test those patients. And on the same token, we want to be able to give the patients who really are at a higher risk that information so that they can use that to formulate their plans with their doctor.
What does a person who finds out they are at a higher risk, what can they do?
Really what they should do is be followed more often. Depending on what their pap test shows as well might change what the doctor decides to do for them. But knowing that they have that virus they are going to want to see if they persist to have that virus over the next few years.
Most women will clear the virus on their own, they have a healthy immune system. So not only knowing that you have the virus, but that the virus is persistent, is what’s important to the development of cervical cancer.
You mentioned a great number of the population does have the HPV virus and there is a push to vaccinate, how important is the vaccination still?
The last I read the uptake of the vaccination in the U.S. was around 30-40% so that’s pretty low. We definitely want to try and get people to go in that direction and get the preventative vaccination. We know now, there is new data, that that is safe for at least 10 years. So we know that we are going in the right direction with the idea of vaccinating for this virus.
With advances in genetic testing, is IU Health is on the forefront?
Cancer care in general is changing. We don’t always want to know what type of cancer you have but what is driving that cancer. Just learning more about the HPV virus and who carries it, what ethnic group is carrying it, that is evolving as time goes on as well. So maybe we’ll find out that 16-18 isn’t the goal for everyone. We hope that maybe by providing this information we can more long term studies and maybe there are other ethnic groups that need to be looked at differently.
IU Health spokeswoman Danielle Sirilla says women getting their regular pap test with an IU Health primary care physician will automatically get screened.
“The HPV test is being done automatically when medically appropriate, in tandem with pap tests,” Sirilla says. “The tests are offered at IU Heath facilities across the state, and samples are sent to the pathology lab in Indianapolis to be tested. Women who are interested in this testing should schedule a pap test with their IU Health primary care physician or OBGYN.”
 DONATE
DONATE








 Support WFYI. We can't do it without you.
Support WFYI. We can't do it without you.