
Paul Gakpo (second from the left) lives in Kentucky with his wife, Michelle (far right) and son, Louis. The family poses for a photo outside their home with Pauls mother, Philomena, in May.
Jacob Dean / Side Effects Public MediaOne night when Paul Gakpo was 9 months old, he fell sick and wouldn’t eat. His parents grew worried and rushed him to a nearby hospital the next morning.
It was 1984. The doctors figured out baby Gakpo’s red blood cells were changing from the typical doughnut shape into the shape of a half moon, and what he was experiencing was a sickle cell disease pain crisis.
“I had some damage done to my feet and my legs, and could have lost my legs,” Paul said. “But luckily they were able to save… my walking ability.”
He was diagnosed with sickle cell disease and placed on a strict regimen of prophylactic penicillin, which is known to reduce the risk of infections that could be life-threatening to children with the genetic disorder. His doctors also had him undergo medical screenings known to improve outcomes for pediatric sickle cell patients.

Paul, now 37, said sickle cell disease was just part of his life growing up in Kentucky. When pain crises hit, he’d end up hospitalized and have to miss school for days at a time.
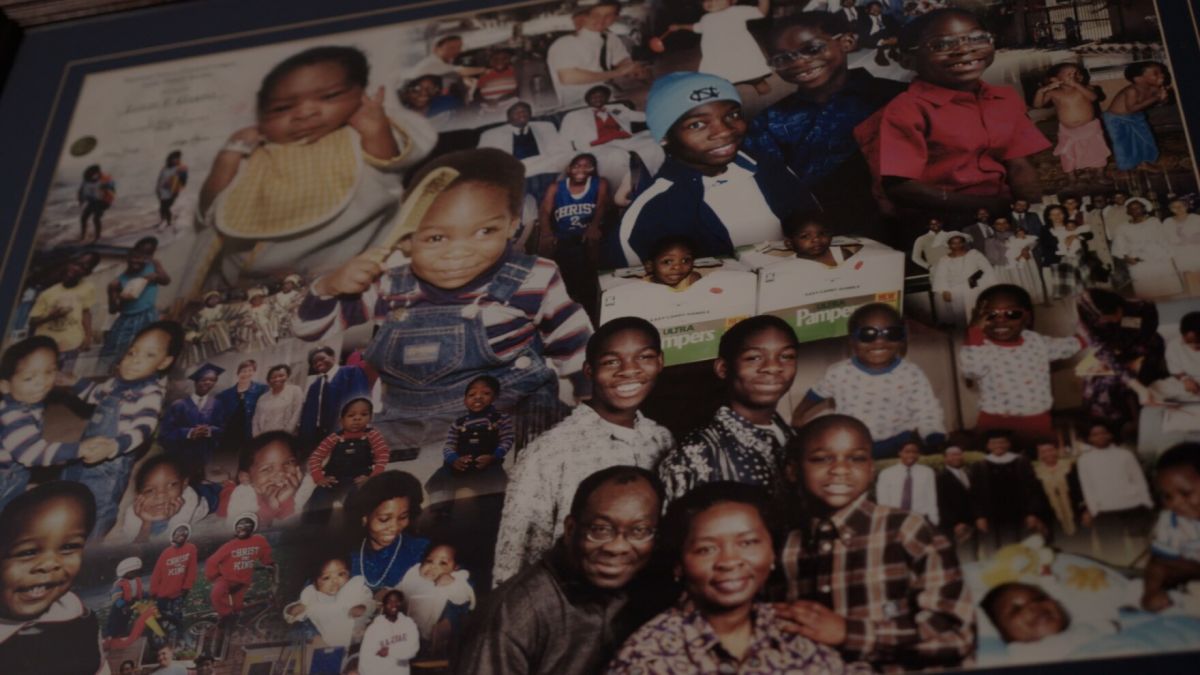
His parents have always been hands-on when it comes to his health. They immigrated to the U.S. before Paul was born — his dad from Ghana and his mom from Nigeria — and used their advanced degrees to land careers in academia. Throughout Paul’s childhood, his mom worked nights as a clinical scientist, and his dad worked the day shift as a professor. This helped ensure someone was always home to take care of sickle cell crises that could strike at any time.
It was tough, but Paul’s mother, Philomena Gakpo, remembers the system was built to help. And they needed a lot of help. Paul’s identical twin brother, Louis, was also diagnosed with sickle cell disease and the two took turns landing in the hospital due to their illness.
“One goes in, then he comes out [and] the other one follows. So we were in the hospital like all the time,” Philomena said. “We had very good, compassionate pediatric physicians… We didn't really know what we were doing, but we had a lot of support.”
For decades, sickle cell was considered a pediatric disease because it claimed the lives of so many young children. In 1970, more than 1 in 4 children born with sickle cell anemia in the U.S. could expect to die before turning 5. This changed when Congress took action to invest millions of dollars to establish sickle cell centers for kids and do more research.
Death rates for children decreased by 68 percent in two decades. For the first time, the vast majority of sickle cell patients were surviving well into adulthood.
That also meant more sickle cell patients outgrew pediatric care and found themselves faced with a system not designed to meet their needs. Federal funding infusions led to the creation of 168 pediatric sickle cell programs across the country, compared to only 49 sickle cell centers for adults.
So while the situation improved dramatically for children, the same cannot be said of adults with the illness. One peer-reviewed study examining death rates of sickle cell patients between 1979 and 2005 found that while child death rates plummeted during that period, adult death rates increased 1 percent every year.
Despite their best efforts, the Gakpos would find their family represented in these heartbreaking statistics.
An unpredictable illness with many uncertainties
When the Gakpo twins turned 18, they moved away from their parents — and out of the pediatric system that had cared so well for them.
“They got to the adult stage with no transition. And then they were out of the house too,” Philomena said.
That came at a cost for Louis Gakpo. His health took one blow after another in the years that followed.
When Louis went to the dentist for a wisdom tooth extraction, he ended up in the ICU for an 11-day stay due to complications from the surgery. While tooth extraction is an outpatient procedure for most, people with sickle cell need inpatient aftercare. Philomena said that didn't happen for Louis, since the dentist did not coordinate with Louis’s hematologist.

A few months later, Philomena said Louis wasn’t feeling well, but his sickle cell specialist wasn’t available. So he went to his primary care provider. Without specialized doctors coordinating his care, she said things went downhill, fast.
Louis Gakpo died in 2004. He was 20 years old.
“I was the last person who saw him,” Philomena said. “He died from complications of sickle cell. He had pneumococcal sepsis, which means he [had] been sick for a few days.”
Many of the challenges faced by people with sickle cell disease can be traced back to systemic racism. The vast majority of sickle cell patients in the U.S. are Black. The disease receives a fraction of the federal and philanthropic dollars that other less-common genetic disorders receive.
This contributes to lack of data and understanding of many sickle cell complications, and a shortage of sickle cell specialists in many parts of the country.
The adult sickle cell system is tough to navigate alone. And to make matters worse, some sickle cell patients have silent brain strokes over the years that can cause cognitive challenges.
“These can all affect memory and planning and the ability for patients to organize their medications and take them on a regular basis," said Dr. Brandon Hardesty, a sickle cell disease hematologist at the Indiana Hemophilia and Thrombosis Center.
The ideal approach to caring for sickle cell patients, he said, is a holistic one, involving a social worker and a psychologist. Such care is often only possible in comprehensive sickle cell centers.
But most sickle cell patients don’t have access to those centers. So when they transition from pediatric to adult care, they often do so without that added layer of support.
‘When I show up at the hospital, I’m scared’
For sickle cell patients, pain crises — the hallmark of the disease — can happen at any time and frequency. Some people experience few pain crises during childhood, and then find sickle cell complications ramp up as they age.
Even with robust pediatric sickle cell care, many families stop seeing specialists if they find the child’s symptoms become manageable, said Dr. Julie Kanter, co-director of the Lifespan Comprehensive Sickle Cell Center at the University of Alabama.
Others drop off from pediatric care due to structural barriers.
“So they haven't seen their hematologist since they were 10, and they start having sickle-cell-related issues when they're 18 or 19,” Kanter said. At that point, they may struggle to find a provider willing to take them on.
Then when crises arise, she said, they may have no choice but to see a non-specialist, like a family medicine physician or an emergency department doctor, who may put them on high doses of opioids for long-term use without addressing the underlying complications of their disease.
“The idea that anyone should be able to treat sickle cell disease is as ridiculous to me as ‘anyone should be able to treat breast cancer,’” Kanter said.
By the time someone in this position connects with an adult sickle cell hematologist, they’ve lost several years of care, Kanter said, “and unfortunately, often [have] multiple complications that sometimes could have been prevented.”
Negative prior experiences with health care providers can also keep adults with sickle cell from seeking medical attention when they need it.
It’s not uncommon to find in patients’ medical records notes from previous doctors that come across as disparaging and distrusting of people’s reported experiences, said Dr. Patrick McGann, the director of the combined pediatric and adult sickle cell and hemoglobinopathy program at Rhode Island Hospital and Hasbro Children’s Hospital.
Things like, “patients report 10 out of 10 pain, but they're watching TV …they're joking …they're sleeping,” he said. “This tells you enough of what they're thinking about that pain and how quickly they are going to treat it. And how are they going to interact with that patient.”
Paul Gakpo said there have been times he was suffering through a pain crisis and felt he wasn’t taken seriously by doctors. The thought of going to the hospital causes so much anxiety that he often puts it off as long as possible, opting instead to “tough it out” or try home remedies.
“So when I show up at the hospital, I'm scared,” he said. “I'm fearing for my life at this point, that the only option I have is to go to the emergency room and, you know, hope that I get what I need there.”
Today, Paul lives in Kentucky with his wife and son. He said suddenly losing his twin brother and best friend to a disease they shared was a huge wake-up call.
Ever since Louis’s death, Paul has made sure to always carry around a piece of paper with him. It’s his sickle cell treatment protocol, signed off by his hematologist.
“[When] I get to the ER after they triage me, I just bring out my protocol, … give it to the doctors and, you know, ask them to follow this guideline,” Paul said.
He’s got copies everywhere: in his car, backpack, jacket pockets. Some are worn and tattered from being carted around to so many places.
It’s his way to make sure he’s believed and taken care of, to minimize the chance things could go wrong.
This story comes from a reporting collaboration that includes the Indianapolis Recorder and Side Effects Public Media, a public health news initiative based at WFYI. Contact Farah at fyousry@wfyi.org. Follow on Twitter: @Farah_Yousrym.
Farah’s reporting on sickle cell disease is supported by a grant from the USC Annenberg Center for Health Journalism’s 2022 Impact Fund for Reporting on Health Equity and Health Systems.
9(MDAyMzk1MzA4MDE2MjY3OTY1MjM5ZDJjYQ000))
 DONATE
DONATE








 Support WFYI. We can't do it without you.
Support WFYI. We can't do it without you.