The open enrollment period for people shopping for health insurance on the Affordable Care Act exchanges runs until January 31, 2016.
stock photoIt’s that time of year again: the open enrollment period for people shopping for health insurance on the Affordable Care Act exchanges. Open enrollment started November 1 and runs until January 31, 2016.
If your employer doesn’t provide insurance and you’re not eligible for Medicare or Medicaid, you’re responsible for buying your own insurance. Depending on your household income, you may be eligible for a tax credit – also called a subsidy – to help cover your costs.
In this guide, we’ve compiled what you need to know to get started. And we culled insider advice from two health care experts, Caitlin Priest, Director of Policy and Communication for the advocacy group Covering Kids and Families of Indiana, and J. Hopkins, senior vice president of ClaimAid, a company that works with hospitals and healthcare providers to help enroll their patients in health insurance.
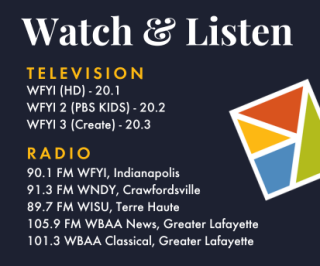
This story was produced by Side Effects Public Media, WFYI’s collaborative health journalism initiative. For more health news, visit sideeffectspublicmedia.org
Menu
2016 Health Insurance Landscape: What’s New This Year
The news for Hoosiers this year looks good. Out of the 37 states on the federal exchange, Indiana is one of only four where the premium price of a benchmark plan – the plan used to calculate subsidies for all plans in the state – is actually going down for 2016. And it’s a significant drop – 12.6 percent.
That means, even if you already have a plan, you should check out what’s available. “Consumers should double check and shop around,” says Priest. “They could be getting a much better deal because that benchmark plan has dropped.”
But don’t go spending your healthcare budget on holiday gifts just yet. According to an analysis by Healthinsurance.org, premium rate changes vary from a 20 percent decrease to a 36 percent increase per plan from 2015 to 2016.
Depending on your income and what kind of coverage you purchase, you could end up paying more every month this year to keep your plan – because a lower-priced benchmark plan means subsidies will also be lower than last year.
And sometimes when an insurer lowers premiums, other costs, like deductibles and copays, may go up. So don’t rush to change plans just because you see one with a lower premium, explains J. Hopkins, vice president of ClaimAid, a company that works with hospitals and healthcare providers to help enroll their patients in health insurance. “The premium may be less, but they’re going to spend more before the insurance kicks in,” Hopkins says.
According to the Department of Health and Human Services, last year, 87 percent of Hoosier consumers who signed up for plans on the exchanges qualified for an average tax credit of $319 per month, and just over half of them paid $100 or less after the subsidy. According to a Gallup poll, the number of Hoosiers without insurance fell from 15.3 percent in 2013 to 11.1 percent at the end of June 2015, a change that experts attribute to the launch of the Affordable Care Act exchange in January 2014, and the expansion of Medicaid (HIP 2.0) earlier this year.
During the 2015 open enrollment period, 216,617 Hoosiers signed up for an exchange plan, about 43 percent of those eligible, according to a Kaiser Family Foundation report. By the end of June this year, however, only 167,261 were still enrolled. Some of those who enrolled for 2015 coverage switched to HIP 2.0 after it opened in February; others got jobs and moved to employer plans, Priest says. But some just didn’t keep up with their premium payments.
It can be a balancing act to select a plan that you fit into your monthly budget and get the care you feel you need. “The ACA took a giant leap forward in helping people get affordable coverage,” Priest says. “But we're not there yet. This is by no means a solved problem.”
Whichever plan you select, it’s certainly better than nothing. Most Hoosiers are required to have health insurance or pay a penalty.
Getting Started: Your Basic Questions Answered
How do I know if I’m eligible for subsidies?
The exchange is designed to insure U.S. residents below the age of 65 who are not insured through a job. The government subsidizes the cost of premiums for people who meet certain income requirements.
In Indiana, residents with estimated annual incomes between 138 and 400 percent of the federal poverty level are eligible to receive a subsidy reducing the cost on their monthly premium. For a single adult, that means anyone earning between $16,242 and $47,080. If you make between 100 and 250 percent of the poverty level you may qualify for additional subsidies if you purchase a silver-level plan.
If you expect to make more than four times the poverty level, you will not receive a subsidy, but you may still purchase health insurance through the exchange – and you’ll have to pay a penalty if you go uninsured.
If your employer offers you insurance, you may opt to purchase a marketplace plan, but you probably won’t receive a subsidy.
I’m not sure if I need Obamacare or public insurance like Medicaid or HIP? How do I know?
If you expect your household income next year will be below 138 percent of the poverty level ($16,242 for individuals), if you are pregnant, or if you are disabled, you may qualify for Indiana’s public insurance programs, including Hoosier Healthwise, traditional Medicaid or the Healthy Indiana Plan (HIP). Learn more about the different programs available here. For a list of poverty guidelines based on family size, click here.
If you’re enrolled in Medicare you can’t purchase a plan on the marketplace. However, if you’re eligible for Medicare but not enrolled, you may choose a Marketplace plan instead.
What’s the deadline to apply?
The last day for open enrollment is January 31. But if you want to get new coverage starting January 1, you need to apply by December 17. For coverage starting February 1, apply by January 15. Plans purchased between January 16 and 31 take effect on March 1. These deadlines apply whether you are enrolling on the marketplace for the first time, or switching plans.
I already have a plan I purchased last year on the exchange — what happens if I do nothing?
You’ll be automatically reenrolled in the same plan as of January 1. You should receive a letter from your insurer detailing any rate changes for 2016. If you haven’t, that information should also be available on the insurer’s website.
Where do I apply?
Since Indiana does not run its own healthcare exchange, Hoosiers can apply on the federal exchange via healthcare.gov. There are trained and certified assisters who can help you located throughout the state – find more information below under Where can I get help?
Are all the same plans available across the state?
Health insurance plans vary from county to county. Browse plans available to you by entering your zip code on Healthcare.gov, or on sites like Healthpocket.com, or Healthinsurance.org. Enter your zip code to see the plans available in your area. There are eight insurance providers operating in Indiana’s marketplace and each offers several plans.
Read more: 2016 individual marketplace coverage in Indiana by carrier
Insurance plans are also categorized by network type. A preferred provider organization (PPO) allows for the most freedom in choosing providers. And exclusive provider organization (EPO) is the narrowest – it only covers care within one health network. You can learn more about network types here.
Silver, Gold, Bronze – it sounds like the Olympics. What do I need to know about the cost categories?
Plans on the healthcare exchange are organized into “metal” categories: Platinum, Gold, Silver and Bronze – each representing a different cost structure. Platinum plans have the highest premiums and the lowest deductibles and other out-of-pocket costs. Bronze plans have the reverse: low premiums and high out of pocket costs.
If you’re 29 or younger or qualify for a hardship exemption, you can buy a very low-premium, high-deductible plan called a catastrophic plan –which pays for three primary care visits, preventive care, and emergency care. (Young folks up to age 26 can stay on a parents’ plan, which may offer better coverage).
What happens if I don’t buy health insurance?
While there are some exemptions –for things like losing a job and other hardships – the rule is that people who have gone without coverage will have to pay a penalty when they file their 2016 tax return. The penalty is going up this year: to 2.5 percent household income or $659 per adult and $347.50 per child under 18 – whichever is higher. And if you end up in the emergency room or need surgery, you can expect the bill to be quite a bit higher.
Choosing A Plan: Consider These Four Important Factors While Shopping For A Plan
1. How much do I use healthcare?
Priest and Hopkins both say it’s important to consider how much you currently use health care. Ask yourself questions like “How often do you visit the doctor? What are your healthcare expenses like? Are you someone with a complex health condition? Do you require specialty care?” says Priest.
Under the Affordable Care Act, insurers can no longer charge more or deny coverage to people with pre-existing conditions. But people with conditions that require care do end up paying more than those who rarely go to the doctor.
“For some folks they might make the decision, ‘I'm gonna buy the cheapest possible plan. I'm worried about spending a lot of money every month, so I want to go cheap cheap cheap,’” says Priest. “That may not be the best deal for you. You may be penny wise and pound foolish, saving money on the front end, but then finding that you have services that aren't covered.”
Hopkins says if you see a doctor for non-preventive care three or more times a year, it makes financial sense to purchase a silver or gold plan.
However, if you’re healthy and only see the doctor once or twice a year, a bronze plan might be right for you. Every plan on the marketplace covers preventive care and emergencies.
2. Can I keep seeing the doctors I like?
When considering a plan, search the insurer’s website or call to see if your doctors are in-network. To make doubly sure, also contact each doctor’s office with the specific name of the plan you’re interested in. Just because your podiatrist accepts plans from Anthem, for example, does not mean she accepts all Anthem plans.
3. How much will my prescriptions cost?
Each plan has its own formulary, says Hopkins, - a list of how much it will pay for different types of drugs. Insurers are required to make their formularies on their websites. Check the formulary for the plan you are considering to see if they cover—and how much they cover—for medications you use regularly.
4. How much will I earn next year?
Estimating your income can get a little tricky, says Hopkins. You have to come up with a number for how much monthly income you expect to make in 2016. Why do you need to estimate your future income instead of putting down the amount you earned last year? Because the subsidies provided by the federal government are really tax credits. If your final income is higher than you estimated, you will have to pay back the difference on your 2016 tax return. If it’s lower than you expected, you’ll get the difference back when you file. Healthcare.gov provides some tips on how to calculate expected income here.
You’ll also have to know how many dependents, if any, you want to place on the plan. Depending on your income, your children might get a better deal by being insured through a spouse, or they might be eligible for Medicaid or Hoosier Healthwise.
Need more help? Find Local, Free Advice, In Person Or Over The Phone
This stuff is complicated. Luckily, there are people ready to help. Two kinds actually --navigators and brokers.
Health insurance navigators (also called assisters) are required to be unbiased – a health insurance company can’t pay them to do their job. They’re trained and certified on the state or federal level. Indiana doesn’t prohibit navigators from charging a fee, but most are available to consumers for free, says Hopkins. They’re required to be knowledgeable about both the Affordable Care Act exchange, and public insurance like HIP and Medicaid. “We can say there's something available for almost everyone,” says Priest, whose organization Caring for Kids and Families has navigators on staff. “No matter where your income is, we can help you figure out the plan that's right for you.”
The Indiana Department of Insurance maintains a database of Indiana certified navigators listed by county. If you’re an Indiana resident, you can work with a navigator in any county.
Private insurance brokers and agents, who are paid by insurance companies, can also help you select a plan on the exchange.
You can find a directory of local assisters, as well as a list of agents and brokers, at localhelp.healthcare.gov.
Have you enrolled on the insurance exchange? Tell WFYI about your experience. Leave a note on our Facebook page or tweet @WFYInews with the hashtags #openenrollment #Indiana
 DONATE
DONATE








 View More Articles
View More Articles




 Support WFYI. We can't do it without you.
Support WFYI. We can't do it without you.